Dental implants have revolutionized tooth replacement, providing a durable and aesthetically pleasing solution for those with missing teeth.
However, the success of dental implants often depends on the quality and quantity of the jawbone into which they are placed. This is where bone grafting plays a crucial role.
Understanding the role of bone grafting in dental implants is essential for anyone considering this tooth replacement option.
Table of content
Understanding Dental Implants
Dental implants are artificial tooth roots, usually made from titanium, surgically placed into the jawbone. They provide a strong foundation for fixed or removable replacement teeth that match natural teeth.
Dental implant surgery involves multiple stages, including the initial consultation, surgical placement, healing and osseointegration (where the implant fuses with the bone), and the final restoration.
Why Bone Grafting is Necessary
Bone grafting is often necessary to repair bone loss that can occur after tooth extraction or due to periodontal disease. When a tooth is lost, the surrounding bone resorbs or shrinks because it no longer supports it.
Bone grafting supports dental implants by adding volume and density to the jawbone, ensuring a stable and long-lasting implant placement.
The Role of Bone Grafting in Dental Implants
Bone grafting plays several critical roles in the dental implant process:
Restoring Lost Bone Volume: Bone grafting compensates for bone loss due to tooth extraction, periodontal disease, or trauma. This restoration is crucial for providing a solid foundation for the dental implant.
Supporting Implant Stability: Adequate bone volume is essential for the stability and integration of the dental implant. Bone grafts ensure enough bone to support the implant and promote successful osseointegration.
Enhancing Aesthetic Outcomes: Bone grafting restores the natural contours of the jawbone, helping achieve a more natural appearance for the final restoration and ensuring that the implant blends seamlessly with the surrounding teeth.
Preventing Future Bone Loss: Bone grafting not only restores current bone volume but also helps prevent further bone resorption, maintaining the structural integrity of the jaw over time.
Types of Bone Grafts
Several types of bone grafts can be used in dental implant surgery, depending on the specific needs of the patient:
Autografts: These grafts use bone harvested from another part of the patient’s body, such as the hip or another part of the jaw. They are the gold standard because they contain living bone cells and growth factors that promote new bone growth.
Allografts: Allografts use bone from a human tissue bank, typically donated by cadavers. The bone is thoroughly processed to ensure safety and compatibility. This option avoids needing a second surgical site in the patient’s body.
Xenografts: Xenografts use bone from an animal source, usually bovine (cow) or equine (horse). The bone is processed to remove all organic material, leaving a mineral scaffold that supports new bone growth.
Alloplasts: These grafts use synthetic materials, such as calcium phosphate or hydroxyapatite, to create a scaffold for new bone growth. Alloplasts are biocompatible and can be used alone or with other grafting materials.
The Bone Grafting Procedure
The bone grafting procedure involves several steps, each crucial for ensuring the success of the dental implant:
Consultation and Planning: The process begins with a thorough evaluation by an oral surgeon or dental specialist. This includes medical history review, oral examination, and imaging studies (such as X-rays or CT scans) to assess bone volume and quality.
Preparation: Depending on the type of graft, the preparation may involve harvesting bone from another part of the patient’s body or preparing donor or synthetic materials.
Anesthesia: Local anesthesia is typically used to numb the area, though sedation or general anesthesia may be offered for more complex procedures or anxious patients.
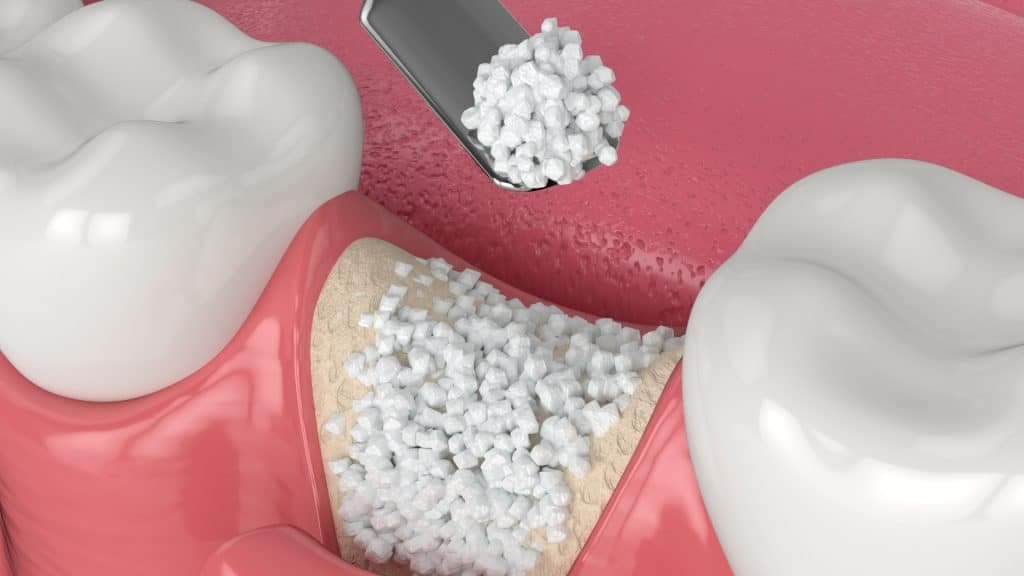
Surgical Procedure: The oral surgeon incurs the gum tissue to expose the underlying bone. The graft material is then placed where bone augmentation is needed. This can be in the tooth socket after extraction, along the bony ridge, or in the sinus cavity (for sinus lift procedures).
Stabilization: The graft material is stabilized using membranes or screws, ensuring it remains in place during the healing process. The gum tissue is then sutured back over the graft.
Healing: The healing process can take several months, during which the graft material integrates with the existing bone and promotes new bone growth. Patients are typically advised to follow specific post-operative care instructions to ensure successful healing.
Post-Operative Care and Healing
Proper care after the bone grafting procedure is crucial for successful healing and integration. Patients should follow their oral surgeon’s instructions, which may include:
- Avoiding Certain Foods: Patients may need to eat soft foods and avoid chewing on the graft site to prevent displacement or damage to the graft material.
- Oral Hygiene: Maintaining good oral hygiene is essential to prevent infection. This includes gentle brushing and rinsing with antimicrobial mouthwashes.
- Medications: Pain medications and antibiotics may be prescribed to manage discomfort and prevent infection.
- Follow-up appointments: Regular follow-up appointments are necessary to monitor healing and address complications.
Factors Influencing Bone Grafting Success
Several factors can influence the success of bone grafting for dental implants:
Bone Quality and Quantity: The condition of the existing bone is a primary determining factor for graft success. Adequate bone volume and healthy bone tissue are crucial for successful integration.
Patient Health: Health, including diabetes or osteoporosis, can affect healing and graft success. Patients are advised to manage any chronic conditions and maintain a healthy lifestyle.
Oral Hygiene: Proper oral hygiene practices are essential to prevent infection and ensure successful healing. Patients must maintain oral health before, during, and after the grafting procedure.
Grafting Material: The grafting material used can impact the procedure’s success. Autografts generally have the highest success rates due to their compatibility and growth potential, while synthetic grafts offer convenience and eliminate the need for a second surgical site.
The Role of Bone Grafting in Specific Dental Implant Scenarios
- After Tooth Extraction: When a tooth is extracted, bone loss can occur in the socket, decreasing bone volume. Ridge preservation techniques involve placing a bone graft in the extraction site to prevent bone resorption and maintain the socket’s shape for future implant placement.
- In the Upper Jaw: The upper jaw often requires bone grafting due to sinus cavities, particularly in the molars and premolars. A sinus lift procedure involves elevating the sinus membrane and placing a bone graft to create a stable foundation for dental implants.
- Periodontal Disease: Periodontal disease can cause significant bone loss around the teeth, affecting the jawbone’s ability to support dental implants. Periodontal bone grafting can restore lost bone and provide a stable foundation for implant placement.
Advances in Bone Grafting Materials and Techniques

The field of bone grafting for dental implants has seen significant advancements in materials and techniques, enhancing the success rates and outcomes for patients:
Synthetic Bone Grafting Materials: Advances in synthetic materials, such as bioactive glass and calcium phosphate, have improved the predictability and success of bone grafting procedures. These materials can stimulate bone growth and scaffold new bone cells.
Growth Factors and Stem Cells: Growth factors and stem cells can accelerate healing and enhance bone regeneration in bone grafting. These biological agents can be combined with grafting materials to promote successful bone healing and integration.
Minimally Invasive Techniques: Advances in surgical techniques have led to minimally invasive approaches for bone grafting, reducing patient discomfort and recovery time. These techniques include using smaller incisions and precise placement of graft materials.
Potential Complications and Risks
Like any surgical procedure, bone grafting carries potential risks and complications, including:
- Infection: Infection at the graft site can occur without proper hygiene.
- Graft Rejection: Although rare, the body can reject the graft material, leading to graft failure.
- Pain and Swelling: Following the procedure, patients may experience pain and swelling, which medications can manage.
- Failure to Integrate: In some cases, the graft material may not integrate with the existing bone, requiring additional procedures.
Conclusion
Bone grafting plays a vital role in the success of dental implants, providing the necessary support and stability for long-term implant function.
Understanding the importance of bone grafting, the types of grafts available, and the procedures involved can help patients make informed decisions about their dental implant treatment.
Zoom Clinic is committed to providing personalized treatment plans that address each patient’s unique needs. Our experienced team of oral surgeons and dental specialists utilizes the latest advancements in bone grafting materials and techniques to ensure successful outcomes.
If you are considering dental implants and have concerns about bone volume or quality, schedule a consultation with us to explore your options and achieve a healthy, beautiful smile.
Get the special offer today from Zoom Clinic
FAQs About Bone Grafting in Dental Implants
What is bone grafting, and why is it necessary for dental implants?
Bone grafting is a surgical procedure that involves adding bone or bone-like materials to the jaw to increase bone volume and density. It is necessary for dental implants when there is insufficient bone to support the implant, often due to bone loss from tooth extraction, periodontal disease, or trauma.
What types of materials are used in bone grafting?
Materials used in bone grafting include autografts (bone from the patient’s own body), allografts (donor bone from a human tissue bank), xenografts (bone from animal sources, usually bovine or equine), and alloplasts (synthetic materials like calcium phosphate).
Is bone grafting painful?
Bone grafting is typically performed under local anesthesia so patients do not feel pain during the procedure. Post-operative discomfort can usually be managed with over-the-counter pain medications, and most patients report only mild to moderate discomfort during the healing process.
How long does it take to recover from a bone grafting procedure?
The initial healing period for a bone grafting procedure is typically a few weeks, but fully integrating the graft material with the existing bone can take several months. Your oral surgeon will provide specific post-operative care instructions to ensure proper healing.
Are there any risks or complications associated with bone grafting?
Like any surgical procedure, bone grafting carries potential risks, including infection, graft rejection, pain, swelling, and failure to integrate with the existing bone. However, these rare complications can often be managed effectively with proper care and follow-up.
How do I know if I need a bone graft for dental implants?
During your consultation, your oral surgeon or dental specialist will evaluate your jawbone’s condition using X-rays or CT scans. If insufficient bone supports an implant, bone grafting is recommended to create a stable foundation.
Can bone grafting be done at the same time as dental implant placement?
Bone grafting and dental implant placement can sometimes be done simultaneously. However, this depends on the extent of bone loss and the type of grafting material used. Your oral surgeon will determine the best approach based on your specific needs.
How do I care for my mouth after a bone grafting procedure?
After a bone grafting procedure, follow your oral surgeon’s instructions, which may include eating soft foods, avoiding chewing on the graft site, maintaining good oral hygiene, and attending follow-up appointments to monitor healing.
Will my insurance cover the cost of bone grafting?
Insurance coverage for bone grafting varies depending on your insurance plan and the specific circumstances of your treatment. Discussing coverage options with your insurance provider and dental clinic is best.
What is the success rate of bone grafting for dental implants?
The success rate of bone grafting for dental implants is generally high, mainly when performed by an experienced oral surgeon and followed by proper post-operative care. Success depends on the patient’s overall health, oral hygiene, and adherence to follow-up care instructions.
Related Articles:
Dental Implants Maintenance: Keeping Your Smile Healthy and Bright
Dental Implants for Multiple Missing Teeth: Solutions and Strategies


